There are various treatments for prostate cancer. The treatment that’s best for each man depends on several factors. These include how fast the cancer is growing, how much it has spread, your age and life expectancy, as well as the benefits and the potential side effects of the treatment. The most common treatments for prostate cancer include the following:
Surgery (Radical prostatectomy)
Surgical removal of your prostate gland, called radical prostatectomy, is used to treat cancer that’s confined to the prostate gland. During this procedure, the surgeon completely removes the prostate and nearby lymph nodes, if necessary. The advantage of this operation is that the tumour (and prostate) is removed from the body which patients often find more reassuring than treatments that are done by leaving the prostate in the patient.
There are four ways to do this:
- Robot-assisted laparoscopic radical prostatectomy (RALRP):
The development of Robotic Assisted Laparoscopic Prostatectomy has transformed the traditional thinking and approach to surgery of the prostate. It has given surgeons a minimally invasive way to perform the same maneuvers that they did with their hands in the open operation. Movements are fully intuitive, instruments are articulated, and the vision is extremely magnified and projected in 3D. For further description please refer to section on robotic surgery.
- Laparoscopic radical prostatectomy: this technique was pioneered in the 1990’s in France and set the benchmark for minimally invasive radical prostatectomy. The operation is extremely difficult to perform because in laparoscopy, for all surgical areas, the instruments are long, rigid and movements are counterintuitive. However, in very skilled hands, there is little difference between laparoscopic radical prostatectomy and robotic assisted laparoscopic radical prostatectomy.
In learning the pure laparoscopic method the surgeon has to perform considerably more cases than the robotic surgeon to achieve the equivalent level of competence. Hence there has been widespread and rapid development of robotic surgery whereas laparoscopic radical prostatectomy is performed by a select few, and becoming redundant in many hospitals.
- Open radical prostatectomy: Historically this method was the standard operation. Its results have set very high standards in terms of cancer control, continence and nerve sparing in the best units. However, the laparoscopic and robotic approaches have shown in studies that they are equivalent in outcomes .In many series there are lower positive margin rates as well as better continence and potency rates, but its hard to prove that when comparing each procedure head to head. If one considers the obvious patient benefits there is little justification to have and open radical prostatectomy if one can have a minimally invasive operation performed by a surgeon with the requisite skills.
- Perineal Prostatectomy. In this approach an incision is made between your anus and scrotum. There’s generally less bleeding with perineal surgery, and recovery time may be shorter, especially if you’re overweight. With this procedure, the surgeon isn’t able to remove nearby lymph nodes. Relatively few surgeons have trained in this method and its potential popularity has been thwarted by the development of robotics and laparoscopy.
Side effects of radical prostatectomy can include:
- Bladder control problems (urinary incontinence). With robotic prostatectomy there might be a small degree of urine leak which can last for weeks or even months, but most men eventually regain bladder control. Often the incontinence is “stress incontinence”, meaning they’re unable to hold urine flow when their bladders are under increased pressure. This can happen when you sneeze, cough, laugh or lift something heavy. In rare cases, urinary incontinence doesn’t get better and surgery is needed to help correct the problem.
- Erectile dysfunction. The nerves that supply the penis to achieve erection are attached to the sides of the prostate and therefore can be damaged during the prostate removal. The enhanced visibility and magnification in robotic surgery helps in identifying the nerve bundle and in good hands results of maintaining potency are excellent. Most men who are 40 – 60 yrs who have nerve-sparing surgery are able to achieve spontaneous erections afterwards; and even some men in their 70s are able to maintain normal sexual function. Men who had trouble achieving or maintaining an erection before surgery have a higher risk of being impotent after the surgery. The recovery of erections can take up to two years and in the meantime patients are likely to need tablets and /or vacuum pump / injections in to the penis to get erections in that time. Some patients will inevitably need these options permanently.
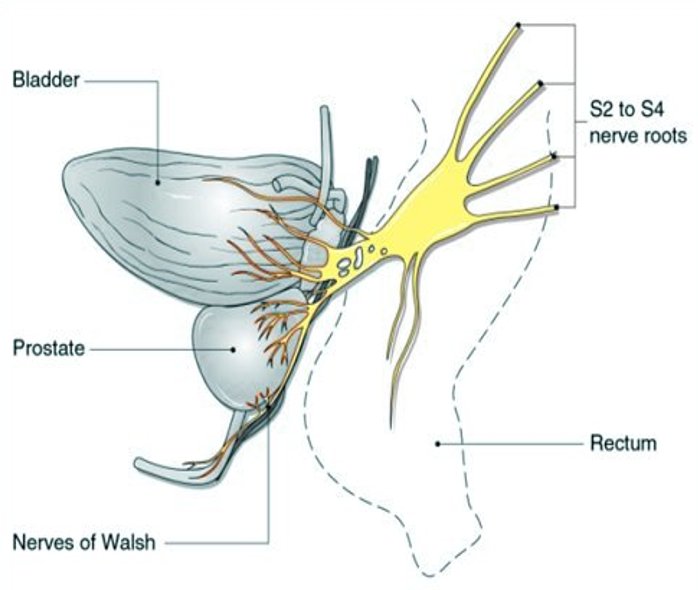
Showing how the of the nerves of erection are attached to the prostate.
External beam radiation therapy (EBRT)
External beam radiation treatment uses high-powered X-rays to kill cancer cells. This type of radiation is effective at destroying cancerous cells, but it can also scar adjacent healthy tissue. The treatment is administered under the auspices of a Clinical Oncologist.
The first step in radiation therapy is to map the precise area of the body that needs to receive radiation. Computer-imaging software helps the doctor find the best angles to aim the beams of radiation. Precisely focused radiation kills cancer in the prostate while minimizing harm to surrounding tissue.
Treatments are generally given five days a week for about eight weeks. Each treatment appointment takes about 10 minutes. However, much of this is preparation time – radiation is received for only about one minute. One doesn’t need anesthesia with external beam radiation, because the treatment isn’t painful.
The treatments are done with a full bladder. This will push most of the bladder out of the path of the radiation beam. A body supporter holds one in the same position for each treatment. Ink marks on the skin help guide the radiation beam, and small gold markers may be placed in the prostate to ensure the radiation hits the same targets each time. Custom-designed shields help protect nearby normal tissue, such as your bladder, erectile tissues, anus and rectal wall.
EBRT can cause mild side effects, but in most cases they disappear shortly after the course of treatment is finished.
Side effects of EBRT can include:
- Urinary problems. The most common signs and symptoms are urgency to urinate and frequent urination. These problems usually are temporary and gradually diminish in a few weeks to months after completing treatment. Long-term problems are uncommon.
- Loose stools, rectal bleeding, discomfort during bowel movements or a sense of needing to have a bowel movement (rectal urgency). In some cases these problems persist for months after treatment, but they improve on their own in most men. If one does have long-term rectal symptoms, medications can help. Rarely, men develop persistent bleeding or a rectal ulcer after radiation. Surgery may be necessary to alleviate these problems.
- Sexual side effects. Radiation therapy doesn’t usually cause immediate sexual side effects such as erectile dysfunction, but the development of erectile problems is often gradual over a year post treatment.
Radioactive seed implants ( Brachytherapy)
Radioactive seeds implanted into the prostate have gained popularity in recent years as a treatment for prostate cancer. The implants, also known as brachytherapy, deliver a higher dose of radiation than do external beams, but over a substantially longer period of time. The therapy is generally used in men with smaller or moderate-sized prostates with small and lower grade cancers.
During the procedure, between 40 and 100 rice-sized radioactive seeds are placed in the prostate through ultrasound-guided needles. The implant procedure typically lasts one to two hours and is done under general anaesthesia. Most men can go home the same day or day after the procedure. Sometimes, hormone therapy is used for a few months to shrink the size of the prostate before seeds are implanted. The seeds may contain one of several radioactive isotopes – including iodine and palladium. These seeds don’t have to be removed after they stop emitting radiation. Iodine and palladium seeds generally emit radiation that extends only a few millimeters beyond their location. This type of radiation isn’t likely to escape the body in significant doses. However, doctors recommend that for the first few months the patient stays at least six feet (1.83 meters) away from children and pregnant women, who are especially sensitive to radiation. All radiation inside the pellets is generally exhausted within a year.
Side effects of radioactive seed implants can include:
- Urinary problems. The procedure causes temporary urinary signs and symptoms such as frequent, slow and painful urination in nearly all men. Patients may require medication to treat these signs and symptoms. Some men need medications or the use of intermittent self-catheterization to help them urinate. Urinary symptoms tend to be more severe and longer lasting with seed implants than with external beam radiation.
- Sexual problems. Up to half the men experience gradual erectile dysfunction due to radioactive seed implants.
- Rectal symptoms. Sometimes this treatment causes loose stools, discomfort during bowel movements or other rectal symptoms. However, rectal symptoms from radioactive seed implants are generally less severe than with external beam radiation.
Hormone Therapy
Hormone therapy involves trying to stop the body from producing the male sex hormones testosterone, which can stimulate the growth of cancer cells. This type of therapy can also block hormones from getting into cancer cells. Sometimes doctors use a combination of drugs to achieve both. In most men with advanced prostate cancer, this form of treatment is effective in helping both shrink the cancer and slow the growth of tumours. Sometimes doctors use hormone therapy in early-stage cancers to shrink large tumours so radiation can remove or destroy them more easily.
Some drugs used in hormone therapy decrease the body’s production of testosterone. The hormones – known as luteinizing hormone-releasing hormone (LH-RH) agonists – can set up a chemical blockade. This blockade prevents the testicles from receiving messages to make testosterone. Drugs typically used in this type of hormone therapy include leuprolide (Lupron, Viadur) and goserelin (Zoladex). They’re injected into a muscle or under the skin once every three months. One can receive them for a few months, a few years or the rest of one’s life, depending on the clinical situation.
Other drugs used in hormone therapy block your body’s ability to use testosterone. A small amount of testosterone comes from the adrenal glands and isn’t suppressed by LH-RH agonists. Certain medications – known as anti-androgens – can prevent testosterone from reaching the cancer cells. Examples include bicalutamide (Casodex) and nilutamide (Nilandron). They come in tablet form and, depending on the particular brand of drug, are taken orally one to three times a day. These drugs typically are given along with an LH-RH agonist.
Simply depriving prostate cancer of testosterone usually doesn’t kill all of the cancer cells. Within a few years, the cancer often learns to thrive without testosterone. Once this happens, hormone therapy is less likely to be effective. However, several treatment options still exist, namely Enzalutamide, abiratorone, and Docytaxel chemotherapy. Sometimes, to avoid hormone resistance, intermittent hormone therapy is used. During this type of therapy, the hormonal drugs are stopped after the PSA drops to a low level and remains steady. The patient then needs to resume taking the drugs if the PSA level rises again.
Side effects of hormone therapy can include:
- Breast enlargement (gynaecomastia)
- Reduced sex drive
- Erectile dysfunction
- Hot flushes
- Weight gain
- Reduction in muscle and bone mass
Certain hormone therapy medications can also cause:
- Nausea
- Diarrhea
- Fatigue
- Liver damage
Reports have shown that men who undergo hormone therapy for prostate cancer may have a higher risk of having a heart attack in the first year or two after starting hormone therapy. Therefore careful monitoring of heart conditions is necessary as well as aggressive treatment of any other conditions that may predispose one to a heart attack, such as high blood pressure, high cholesterol or smoking.
Surgery to remove the active portion of the testicles, which produce most of your testosterone, is as effective as other forms of hormonal therapy. Doing this surgery has the advantage of not having to have an injection every three or four months and can be less expensive. The surgery can be done on an outpatient basis using a local anesthetic.
Watchful Waiting/Active surveillance
The PSA blood test can help detect prostate cancer at a very early stage. This allows many men to choose watchful waiting or active surveillance as a treatment option.
In watchful waiting, no medical treatment is provided. Medications, radiation and surgery aren’t used. Watchful waiting may be an option if the cancer isn’t causing symptoms, is small volume and expected to grow very slowly, Generally, this is reserved for older patients who are unlikely to die form the prostate cancer and therefore might never need treatment. In other words many such men will live out their normal life spans without treatment and without the cancer spreading or causing other problems.
Active surveillance is different in that it implies deferred treatment. Hence even a relatively young man can be placed on active surveillance while his cancer is very early stage. Mostly these cancers were found incidentally and have no symptoms and there is a considerably long window of opportunity to treat them, eventually with curative intent. There is a small chance that the cancer can spread in that time though and therefore patients have to be comfortable with this choice and not live with substantial anxiety about the presence of the cancer. Regular follow-up blood tests, rectal exams, MRI’s and possibly biopsies may be performed to monitor progression of the cancer.
Chemotherapy
This type of treatment uses chemicals that destroy rapidly growing cells. Chemotherapy can be quite effective in treating prostate cancer, but it can’t cure it. Because it has more side effects than hormone therapy does, chemotherapy is reserved for men who have hormone-resistant prostate cancer that has spread to other parts of the body.
Cryotherapy
This treatment is used to destroy cells by freezing tissue. Original attempts to treat prostate cancer with cryotherapy involved inserting a probe into the prostate through the skin between the rectum and the scrotum (perineum). Using a rectal microwave probe to monitor the procedure, the prostate was frozen in an attempt to destroy cancer cells. This method often resulted in damage to tissue around the bladder and long-term complications such as injury to the rectum or the muscles that control urination.
More recently, smaller probes and more-precise methods of monitoring the temperature in and around the prostate have been developed. These advances may decrease the complications associated with cryotherapy, making it a more effective treatment for prostate cancer. Although progress continues, more time is needed to determine how successful cryotherapy may be as a treatment for prostate cancer.
Gene Therapy and Immune Therapy
In the future, gene therapy or immune therapy may be successful in treating prostate cancer. Current technology limits the use of these experimental treatments to a small number of medical centres.

